Navigate to your symptom
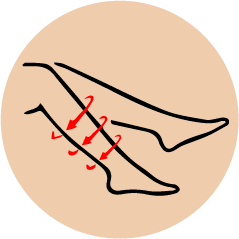
Uncovering vein-related causes of Leg Pain
Discomfort in the legs—such as aching, cramping, or heaviness—can often be a sign of vein disease, a condition that impairs healthy blood circulation. When veins struggle to return blood to the heart, whether due to varicose veins, poor circulation, or blood clots, pressure can build in the lower limbs. This leads to symptoms that may intensify with prolonged sitting or standing. In many cases, elevating the legs brings temporary relief. If left unaddressed, these issues can lead to more serious health concerns.
Causes of Varicose Veins
Varicose veins develop due to increased venous pressure and weak vein walls. Some primary causes include:
- Weak or Damaged valves – Veins have one-way valves to prevent blood from flowing backward. If they become weak, blood accumulates and causes swelling.
- Increased Pressure on the Legs – Prolonged standing, sitting, or excess weight can lead to increased pressure in leg veins.
- Hormonal Changes – Pregnancy, menopause, and birth control pills can affect vein elasticity.
- Genetics – A family history of varicose veins increases the likelihood of developing them.
- Aging – As veins lose elasticity over time, they become more prone to enlargement.
- Lack of Physical Activity – Sitting or standing for long periods slows blood circulation, increasing vein pressure.
Symptoms of Varicose Veins
- Visible, twisted, swollen veins (blue or purple)
- Aching or heaviness in the legs (especially after standing for long periods)
- Burning, throbbing, or cramping sensations
- Swelling in the lower legs and ankles
- Itchy or irritated skin near the veins
- Skin discoloration (in severe cases, brownish or reddish patches may appear)
- Ulcers or open sores (if left untreated)
Types of Varicose Veins
- Trunk Varicose Veins – Large, swollen veins near the skin’s surface.
- Reticular Varicose Veins – Smaller, reddish or blue veins that form a network on the legs.
- Spider Veins (Telangiectasias) – Tiny, web-like veins that appear on the legs or face.
Uncovering vein-related causes of Leg Pain
Discomfort in the legs—such as aching, cramping, or heaviness—can often be a sign of vein disease, a condition that impairs healthy blood circulation. When veins struggle to return blood to the heart, whether due to varicose veins, poor circulation, or blood clots, pressure can build in the lower limbs. This leads to symptoms that may intensify with prolonged sitting or standing. In many cases, elevating the legs brings temporary relief. If left unaddressed, these issues can lead to more serious health concerns.
Common Causes of Leg Pain
Leg discomfort can stem from a variety of vein-related conditions. Below are some of the most common contributors:
- Varicose Veins – These are enlarged, twisted veins typically found in the legs, caused by weakened or faulty valves. They can lead to heaviness, throbbing, and persistent aching in the legs.
- Chronic Venous Insufficiency (CVI) – CVI occurs when the vein walls or valves in the legs are not functioning properly, making it difficult for blood to flow back to the heart. This condition can cause swelling, fatigue, and aching in the lower limbs.
- Deep Vein Thrombosis (DVT) – A serious condition where blood clots form in the deep veins, often in the legs. DVT can lead to swelling, pain, and a feeling of warmth, and poses a risk of complications like pulmonary embolism if left untreated.
- Spider Veins – These are smaller, visible veins close to the surface of the skin. While often considered cosmetic, they can sometimes cause burning, itching, or mild cramping in the legs.
Common Symptoms of Vein-Related Leg Pain
Leg pain due to underlying vein conditions can present in several ways, including:
- Dull, aching discomfort that worsens after long periods of standing or sitting
- Cramping or throbbing sensations, often more noticeable at night.
- Heaviness or fatigue in the legs, especially toward the end of the day
- Swelling in the lower legs, ankles, or feet
- Burning or itching sensations along the veins
- Skin changes, including dryness, redness, or dark discoloration
- Slow-healing wounds or ulcers, typically around the ankles (in advanced cases)
Treatment Options for Vein-Related Leg Pain
We offer state-of-the-art, minimally invasive treatments designed to relieve leg pain caused by poor vein function, restore healthy blood flow, and improve your overall quality of life:
- Radiofrequency Ablation (RFA) – A gentle, heat-based procedure that closes off faulty veins, reducing pain, swelling, and fatigue.
- Ultrasound-Guided Sclerotherapy – A precise injection of a medicated solution into smaller or medium-sized veins, causing them to collapse and fade, relieving cramping and heaviness.
- Varithena® Foam Therapy – A specialized, microfoam injection used to treat larger varicose veins with minimal discomfort, improving circulation and reducing leg aches.
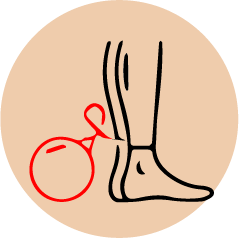
Uncovering vein-related causes of Leg Ulcers

Persistent leg wounds that are slow to heal—commonly known as venous leg ulcers—can be a serious sign of underlying vein disease. When vein valves fail to circulate blood efficiently back to the heart, pressure can build up in the lower legs. Over time, this increased pressure may damage skin tissue and lead to open sores, particularly near the ankles. These ulcers are often accompanied by swelling, skin discoloration, and discomfort. Without proper vein treatment, they may worsen or become infected, making early intervention essential for long-term healing and prevention.
Common Causes of Leg Ulcers
Leg ulcers often result from underlying venous issues that impair proper blood flow and damage surrounding tissues. Below are key vein-related conditions that can lead to the development of leg ulcers:
- Chronic Venous Insufficiency (CVI) – When the veins in the legs fail to return blood efficiently to the heart, pressure builds up and damages the skin over time. This can result in slow-healing wounds, especially near the ankles.
- Varicose Veins – Enlarged, malfunctioning veins can cause increased pressure in the lower legs, contributing to skin breakdown and ulcer formation in severe cases, particularly when left untreated.
- Post-Thrombotic Syndrome (PTS) – A long-term complication of Deep Vein Thrombosis (DVT), PTS can lead to chronic swelling, pain, and skin changes that make the legs more vulnerable to ulceration.
- Venous Hypertension – Elevated pressure within the veins—often due to valve failure—can impair oxygen delivery to skin tissue, triggering inflammation and the development of ulcers.
Common Symptoms of Vein-Related Leg Ulcers
Venous leg ulcers often develop gradually and may be accompanied by several noticeable symptoms, including:
- Persistent sores or wounds, usually near the ankles, that are slow to heal
- Itching, burning, or irritation around the affected area
- Thickened or hardened skin (known as lipodermatosclerosis) near the ulcer site
- Swelling in the lower leg, especially after standing for long periods
- Dark or reddish skin discoloration, often surrounding the wound
- Oozing or crusting wounds, which may produce an unpleasant odor if infected
- Pain or tenderness, particularly when walking or applying pressure to the area
Treatment Options for Vein-Related Leg Ulcers
- Endovenous Radiofrequency Ablation (RFA) : A heat-based treatment that seals malfunctioning veins, relieving venous pressure and supporting ulcer healing from the inside out.
- Ultrasound-Guided Foam Sclerotherapy : A targeted injection of a medicated foam into diseased veins to collapse them, reducing inflammation and improving blood flow to support faster wound recovery.
- Compression Therapy :Medical-grade compression stockings or wraps are used to reduce swelling, enhance circulation, and provide essential support for healing existing ulcers and preventing new ones.
- Wound Care & Debridement : Specialized care for the ulcer itself, including cleaning, dressing, and removal of dead tissue when necessary to encourage healthy skin regrowth.
Uncovering vein-related causes of Skin Discoloration
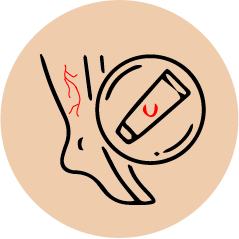
Changes in skin color—especially darkening or reddish patches on the lower legs—can be an early warning sign of chronic vein disease. When veins fail to circulate blood effectively, pressure builds in the surrounding tissue, leading to inflammation and blood pooling. Over time, this can cause hyperpigmentation, usually around the ankles or shins. Affected areas may appear brownish, purplish, or even leathery in texture. These changes often develop gradually and may be accompanied by itching, dryness, or irritation. Without timely vein treatment, skin discoloration can worsen and increase the risk of ulcers or permanent skin damage.
Common Causes of Skin Discoloration
Skin discoloration in the lower legs is often an early sign of venous disease and typically develops due to prolonged pressure and poor circulation. Here are the most common vein-related contributors:
- Chronic Venous Insufficiency (CVI) – When veins struggle to return blood to the heart, blood can pool in the lower legs, leading to inflammation and leakage of red blood cells into the skin. This often causes brownish or reddish patches, particularly around the ankles.
- Varicose Veins – Enlarged, dysfunctional veins can increase local pressure and contribute to skin changes, such as darkening, dryness, or itching. Over time, the skin may become leathery or hardened.
- Post-Thrombotic Syndrome (PTS) – Following a deep vein thrombosis (DVT), long-term vein damage can result in poor circulation, leading to swelling, pigmentation changes, and a higher risk of tissue breakdown.
- Venous Hypertension – Abnormally high pressure in the leg veins can reduce oxygen flow to the skin, triggering chronic inflammation and causing the skin to darken or take on a reddish-purple hue.
Common Symptoms of Vein-Related Skin Discoloration
Skin discoloration caused by underlying venous issues can progress gradually and is often accompanied by other signs of poor circulation, such as:
- Dark, brownish, reddish, or purplish patches on the lower legs, especially around the ankles
- Dry, itchy, or flaky skin in the discolored area
- Thin or fragile skin that may break easily or feel irritated
- Hardening or thickening of the skin (known as lipodermatosclerosis)
- Swelling in the lower legs or ankles, especially after long periods of standing or sitting
- Visible veins or varicose veins near the discolored area
- A feeling of tightness or heaviness in the legs
- Progression to open sores or ulcers in advanced cases
Treatment Options for Vein-Related Skin Discoloration
- Endovenous Radiofrequency Ablation (RFA) :
A thermal procedure that closes damaged veins, reducing venous pressure and helping prevent further skin damage or darkening caused by poor blood flow.
- Ultrasound-Guided Foam Sclerotherapy :
A precise foam injection that collapses problematic veins beneath the skin, improving circulation and gradually reducing pigmentation and inflammation in affected areas. - Compression Therapy :
Medical-grade compression stockings promote proper blood flow, reduce swelling, and support reversal of early skin discoloration by minimizing blood pooling in the lower legs.
- Topical & Supportive Skin Treatments : Moisturizers, anti-inflammatory creams, and barrier-protecting agents can help relieve itching, dryness, and irritation associated with venous skin changes.
- Lifestyle and Preventive Care : Elevating the legs, regular movement, weight management, and avoiding prolonged standing or sitting can all support better vein health and slow the progression of skin discoloration.
Uncovering vein-related causes of Burning/Tingling Sensation

Tingling or burning sensations in the legs can be an early indicator of underlying vein disease. When veins are unable to circulate blood efficiently, pressure and inflammation can affect surrounding nerves and tissues. This impaired circulation may result in sensations such as pins-and-needles, warmth, or a mild burning feeling—especially in the lower legs or feet. These symptoms often develop gradually and may worsen with prolonged standing or sitting. They are commonly accompanied by heaviness, swelling, or visible vein changes. If left untreated, these nerve-related symptoms can progress and may signal advancing venous insufficiency requiring medical attention.
Common Causes of Burning Sensation
Tingling or burning feelings in the legs may be more than just nerve irritation—they can be signs of vein disease affecting circulation and nerve health. Below are common vein-related contributors:
- Chronic Venous Insufficiency (CVI) – When blood doesn’t flow efficiently back to the heart, pressure builds in the veins and surrounding tissues. This can irritate nearby nerves, causing sensations like tingling, burning, or numbness in the legs—especially after standing or sitting for extended periods.
- Varicose Veins – Bulging, weakened veins can press against nearby nerves and lead to discomfort, including mild burning or prickling sensations. These symptoms may be more noticeable at the end of the day or during warm weather.
- Post-Thrombotic Syndrome (PTS) – A long-term complication of deep vein thrombosis (DVT), PTS can cause ongoing pain, swelling, and nerve-related symptoms such as tingling or heat-like discomfort in the lower limbs.
- Venous Hypertension – Elevated pressure inside the veins can impair both blood flow and nerve signaling. This can result in abnormal sensations such as pins-and-needles, burning, or creeping feelings, particularly in the calves and ankles.
Common Symptoms of Vein-Related Tingling / Burning Sensation
Abnormal sensations such as burning or tingling in the legs can be subtle signs of underlying venous insufficiency and are often accompanied by other symptoms of poor circulation, including:
- A pins-and-needles feeling or tingling in the lower legs, feet, or ankles
- A mild to intense burning sensation, especially after long periods of standing or sitting
- Localized warmth or heat-like discomfort in areas with visible veins
- Leg fatigue or a feeling of heaviness, particularly toward the end of the day
- Mild numbness or a “falling asleep” feeling in the legs
- Swelling in the lower legs or ankles, often worsening with prolonged inactivity
- Visible varicose or spider veins in areas experiencing discomfort
- Skin sensitivity or irritation near affected veins
- Progression to skin discoloration or ulceration if the underlying condition is left untreated
Treatment Options for Vein-Related Burning Sensation
- Endovenous Radiofrequency Ablation (RFA) :A heat-based procedure that closes off malfunctioning veins, relieving venous pressure and reducing nerve irritation that often leads to burning or tingling sensations.
- Ultrasound-Guided Foam Sclerotherapy :This targeted foam injection collapses faulty veins, improves blood flow, and helps reduce inflammation and pressure on nearby nerves, easing abnormal sensations in the legs.
- Compression Therapy :
Medical-grade compression stockings help support healthy blood flow, minimize swelling, and alleviate pressure on nerves that may contribute to tingling, prickling, or heat-like discomfort. - Neuropathy-Supportive Care : In cases where nerve sensitivity is present, supportive treatments such as B-vitamin supplements, anti-inflammatory medications, or nerve-calming creams may be recommended alongside vein therapies.
- Lifestyle Modifications : Staying active, elevating the legs, maintaining a healthy weight, and avoiding prolonged standing or sitting can help improve circulation and reduce the frequency of burning or tingling sensations.
Uncovering vein-related causes of Varicose / Spider Veins
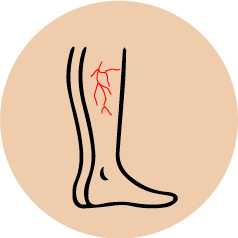
Varicose and spider veins are often visible signs of underlying vein disease. When vein valves weaken or become damaged, they fail to circulate blood efficiently back to the heart. This leads to increased pressure within the veins, causing them to stretch, twist, and become enlarged over time. As a result, varicose veins appear as bulging, rope-like veins beneath the skin, while spider veins show up as fine, web-like networks closer to the surface. These changes typically develop gradually and may be accompanied by symptoms such as heaviness, aching, or burning sensations in the legs. Without treatment, they can progress and contribute to chronic venous insufficiency or skin complications.
Common Causes of Varicose / Spider Veins
Varicose and spider veins often develop due to vein conditions that weaken vessel walls and valves over time. Below are the most common underlying contributors:
- Chronic Venous Insufficiency (CVI) – When vein valves stop functioning properly, blood flows backward and pools in the legs. This added pressure causes veins to stretch and become twisted, resulting in enlarged varicose veins or clusters of spider veins.
- Weak or Damaged Valves – Faulty valves in superficial veins allow blood to leak backward instead of moving toward the heart. Over time, this can cause visible surface veins to expand and branch into web-like spider veins.
- Hormonal Changes – Fluctuations during puberty, pregnancy, or menopause can weaken vein walls and valves, especially in women. This makes varicose and spider veins more likely to form, particularly in the legs or pelvic area.
- Genetic Predisposition – A family history of vein disease or varicose veins significantly increases the likelihood of developing similar issues, even in younger individuals or those with active lifestyles.
- Prolonged Standing or Sitting – Occupations or lifestyles involving long hours on the feet or seated can slow circulation, increasing venous pressure and the risk of vein dilation over time.
- Age-Related Wear – As we age, vein walls naturally lose elasticity and valves weaken, making older adults more prone to both spider and varicose veins—even in the absence of other medical issues.
Common Symptoms of Underlying Vein Disease
Visible vein issues like varicose and spider veins are often more than just cosmetic concerns—they may signal chronic venous insufficiency or impaired circulation. These symptoms tend to develop gradually and may worsen over time:
- Bulging, twisted, or rope-like veins that appear raised on the surface of the skin, most commonly on the legs or behind the knees
- Clusters of small, web-like veins (spider veins) in red, blue, or purple, often seen on the thighs, ankles, or face
- Aching, throbbing, or cramping sensations in the legs, especially after prolonged standing or at the end of the day
- Leg heaviness or fatigue, which may improve with elevation or rest
- Swelling (edema) in the ankles or calves, often worse in the evening or after sitting for long periods
- Itching or irritation around the veins, sometimes misdiagnosed as dry skin or dermatitis
- Skin changes, such as dryness, thinning, dark patches, or leathery texture near the ankles
- Increased warmth or tenderness over the enlarged veins
- Nighttime leg discomfort or restlessness, sometimes linked to vein-related pressure
- Progression to skin ulcers in advanced stages of venous disease, particularly near the inner ankle
Treatment Options for Varicose Veins and Spider Veins
Treatment Options for Varicose Veins and Spider Veins
- Endovenous Radiofrequency Ablation (RFA) : A minimally invasive procedure that uses controlled heat to seal off damaged veins. This reduces venous pressure, improves circulation, and helps veins shrink over time—especially effective for large, bulging varicose veins.
- Ultrasound-Guided Foam Sclerotherapy : A precise injection of medical-grade foam into affected veins causes them to collapse and be naturally reabsorbed by the body. This treatment is ideal for smaller varicose veins and spider veins, and often improves both appearance and symptoms like aching or heaviness.
- Laser Treatments (EVLT or Surface Laser Therapy):
Laser energy is used either internally (endovenous) or externally (surface laser) to target problem veins. This approach is commonly used for smaller veins and spider veins, especially on the face or legs.
- Compression Therapy : Wearing prescription-strength compression stockings helps push blood back toward the heart, reduces swelling, and prevents worsening of visible veins. It also relieves discomfort such as aching or throbbing in the legs.
- Vein Stripping or Microphlebectomy : In more advanced cases, surgical removal of larger varicose veins may be recommended. These procedures are often done under local anesthesia and provide long-term relief for prominent, symptomatic veins.
- Lifestyle Modifications:Daily movement, weight control, leg elevation, and minimizing prolonged standing or sitting can help improve circulation and reduce the formation or worsening of spider and varicose veins.
Uncovering vein-related causes of restlessness in the legs
Restlessness in the legs—often described as an uncontrollable urge to move the legs, especially at night—can be an overlooked sign of underlying vein disease. When vein valves become weak or damaged, they fail to return blood efficiently to the heart. This leads to pooling of blood in the lower legs, causing increased pressure, inflammation, and irritation of surrounding nerves and tissues. Over time, this impaired circulation can trigger sensations such as crawling, tingling, or a deep, uncomfortable urge to move the legs—particularly when sitting or lying down. Restlessness is often worse in the evening or during long periods of inactivity and may be relieved temporarily by movement. These symptoms may develop gradually and are commonly seen alongside other venous issues like swelling, heaviness, or visible varicose and spider veins. If left untreated, chronic restlessness can disrupt sleep and quality of life, and may signal progressing chronic venous insufficiency that requires medical evaluation and care.
Common Causes of Restlessness in the legs
Restless sensations in the legs—especially in the evening or at night—can often be traced back to vein conditions that disrupt healthy circulation. These underlying issues lead to pressure buildup and nerve irritation in the lower limbs, which may trigger an overwhelming urge to move or stretch the legs. Common causes include:
- Chronic Venous Insufficiency (CVI) – When valves in leg veins become inefficient, blood pools rather than returning properly to the heart. This stagnant flow increases pressure and can irritate nerves and tissues, leading to restlessness, discomfort, and a crawling or tingling sensation in the legs—especially at night.
- Elevated Venous Pressure – Persistent pressure in leg veins from poor circulation can result in sensations of internal agitation or discomfort. These feelings are often relieved by movement, leading to frequent tossing, turning, or walking during periods of rest.
- Nerve Irritation from Vein Swelling – As veins expand due to pooling blood, they may compress or irritate surrounding nerves. This can result in odd sensations such as buzzing, prickling, or restlessness that prompt leg movement for relief.
- Hormonal and Physiological Factors – Hormonal fluctuations, especially in women during pregnancy or menopause, can heighten vein sensitivity and exacerbate symptoms like leg restlessness, particularly when combined with fluid retention or weight changes.
- Prolonged Inactivity – Extended periods of sitting or standing can reduce venous return and worsen restlessness. This is especially common in people with sedentary jobs or who travel frequently.
- Genetics and Aging – A hereditary predisposition to vein issues or natural age-related weakening of vein walls and valves may lead to earlier onset or worsening of restless leg sensations due to impaired venous circulation.
Restlessness : A sign of Vein Disease
Restlessness in the legs—especially during the evening or while trying to sleep—can be more than just an annoyance. It may be an early indicator of underlying venous insufficiency, where poor blood flow leads to pressure buildup and nerve irritation in the lower limbs. This discomfort often worsens over time if left untreated.
- An overwhelming urge to move the legs, especially when sitting or lying down
- Creeping, crawling, or tingling sensations in the calves or thighs
- Discomfort that worsens in the evening or during periods of inactivity
- Temporary relief with movement, stretching, or walking
- Heaviness, throbbing, or mild burning accompanying restlessness
- Visible varicose or spider veins in areas with frequent discomfort
- Leg fatigue or aching after long hours on your feet
- Warmth or tightness in the lower legs, particularly near swollen veins
- Disrupted sleep due to frequent leg movement or discomfort at night
- Restlessness paired with swelling, itching, or skin changes in the lower legs
Treatment Options for Restlessness in legs caused by Vein Disease
- Endovenous Radiofrequency Ablation (RFA) : A heat-based procedure that closes malfunctioning veins from the inside. By restoring proper blood flow and reducing pressure in the lower limbs, RFA helps ease nerve-related sensations like restlessness, tingling, and heaviness—especially during inactivity or at night.
- Ultrasound-Guided Foam Sclerotherapy : This targeted, minimally invasive treatment collapses abnormal veins using a specialized medical foam. As faulty veins are absorbed and circulation improves, symptoms such as leg agitation, aching, and an urge to move often diminish.
- Laser Treatments (EVLT or Surface Laser Therapy) : Laser therapy, delivered internally or externally, seals off small problematic veins—improving circulation and reducing nerve irritation. It is especially effective when restless sensations are linked to spider veins or small varicose veins.
- Compression Therapy : Wearing medical-grade compression stockings enhances venous return, relieves pressure buildup, and calms irritated nerves. Regular use can help reduce restlessness, especially when symptoms worsen in the evening or after long periods of standing or sitting.
- Neuromuscular Support & Supplements : In cases where nerve sensitivity plays a role, certain supplements (e.g., magnesium, iron, or B-complex vitamins) may support nerve and vein health. These are sometimes used alongside vein treatments to reduce nighttime discomfort and improve sleep quality.
- Lifestyle Modifications:Simple daily changes like regular walking, leg elevation, staying hydrated, and avoiding prolonged sitting or standing can significantly reduce restlessness. Incorporating gentle stretching or calf exercises before bedtime may also help settle the legs.
Uncovering vein-related causes of heaviness / fatigue in the legs
As a result, the legs may feel tired, achy, or weighed down—even after minimal activity. These symptoms often worsen throughout the day and may improve temporarily with leg elevation or rest. Over time, the added strain on the veins and surrounding tissues can lead to more pronounced discomfort, difficulty with prolonged standing or walking, and reduced stamina.
Heaviness and fatigue in the legs frequently occur alongside other signs of venous insufficiency, such as visible varicose veins, swelling, cramping, or itching. If left untreated, these sensations can interfere with daily activities and may indicate progressing vein dysfunction that warrants professional evaluation and targeted treatment.
Common Causes of Heaviness / Fatigue in the legs
A sense of heaviness, tiredness, or dragging in the legs—especially after standing, walking, or at the end of the day—is often a subtle yet telling indicator of compromised venous health. Several underlying vein-related conditions contribute to this sensation:
- Chronic Venous Insufficiency (CVI) –
When vein valves become weak or fail altogether, they allow blood to pool in the lower legs instead of flowing efficiently back to the heart. This stagnant circulation creates internal pressure, leading to heaviness, aching, and premature muscle fatigue even with light activity. - Venous Hypertension (Elevated Vein Pressure) –
Over time, the buildup of blood in the leg veins increases internal pressure, stretching vein walls and causing discomfort. This pressure overload can weigh down the legs, creating a sensation of fatigue and making movement feel laborious or strained.
- Tissue Congestion from Blood Pooling –
Inefficient venous return results in fluid leakage and mild inflammation in surrounding tissues. This congestion reduces oxygen and nutrient supply to the muscles, contributing to early-onset fatigue, soreness, and a feeling of leg “tightness” or fullness.
- Prolonged Standing or Sedentary Behavior –
People with vein issues often experience worsened heaviness during long periods of standing or sitting. This lack of movement impairs calf muscle function—an essential aid to venous return—leading to sluggish circulation and leg fatigue.
- Hormonal and Physiological Changes –
Pregnancy, menopause, or hormonal therapy can soften vein walls and increase venous pooling, particularly in women. These physiological changes can intensify sensations of heaviness and contribute to leg discomfort.
- Age and Genetics –
As veins lose elasticity with age—or due to inherited vein conditions—valve function declines. The result is a gradual increase in venous pressure and heaviness in the legs, even in the absence of visible varicose veins.
Common Symptoms of Heaviness / Fatigue in the legs
A heavy, tired feeling in the legs—especially after long hours of standing or sitting—can be more than just everyday fatigue. It may signal chronic venous insufficiency (CVI), a condition in which weakened or damaged vein valves fail to circulate blood effectively back to the heart. This leads to pooling of blood, increased pressure in the veins, and muscle fatigue that worsens with time if left unaddressed.
- A persistent feeling of heaviness or dragging in the legs, particularly in the calves or thighs
- Fatigue in the legs that appears early in the day or worsens with minimal physical activity
- Aching, soreness, or a dull throbbing sensation after standing or walking
- Relief when legs are elevated, massaged, or rested
- Swelling in the lower legs or ankles, especially toward the evening
- Visible varicose or spider veins in areas experiencing heaviness
- Tightness or a sense of fullness in the calves
- Legs that feel stiff or sluggish, especially in warmer weather or after inactivity
- Skin changes, such as dryness, dark patches, or itchiness around swollen areas
- Difficulty with prolonged standing or walking due to fatigue or discomfort
Treatment Options for Restlessness in legs caused by Vein Disease
- Endovenous Radiofrequency Ablation (RFA) : A minimally invasive procedure that uses heat energy to seal off damaged veins. This reduces pressure in surrounding veins, relieves leg fatigue, and restores normal blood flow—ideal for patients with chronic heaviness and varicose veins.
- Ultrasound-Guided Foam Sclerotherapy : This technique involves injecting a special foam into the problem veins, causing them to collapse and be reabsorbed by the body. It’s highly effective for treating smaller varicose and spider veins that contribute to leg fatigue or soreness.
- Laser Treatments (EVLT or Surface Laser Therapy) : Laser energy is delivered through a thin fiber inside the vein to close off faulty veins. This promotes better circulation and reduces symptoms like aching, heaviness, and tired legs—especially in those with early to moderate venous insufficiency.
- Compression Therapy : Medical-grade compression stockings help push blood upward from the legs toward the heart. This reduces venous pressure, swelling, and the sensation of heaviness—often recommended as a first-line therapy or to support other treatments.
- Microphlebectomy (Ambulatory Phlebectomy) : A procedure in which visibly bulging veins are removed through tiny skin punctures under local anesthesia. It provides immediate relief from heaviness, fatigue, and discomfort caused by superficial varicose veins.
- Lifestyle Changes and Preventive Measures : Regular physical activity, leg elevation, weight management, and avoiding prolonged sitting or standing can all help ease fatigue and heaviness in the legs. These changes improve circulation and reduce the strain on leg veins.
